Have that conversation on end of life planning
The issue of death and dying is one which we often, as a society find difficult to talk about, particularly with our frail and elderly loved ones. Few of us want to consider the end.
With the pandemic sweeping across the world this year, this issue has been brought into sharp focus for many. A recent survey found that 74% of people had never prepared a statement of their end of life wishes or preferences and only 11% had discussed this with family and friends.
Paul Turley, Commissioning lead for Palliative and End of Life Care, Health and Social Care Board said, “Talking about dying, death and bereavement is often a very delicate conversation to initiate and follow through. If we can support individuals and families to work through the conversations that are needed, this will go a long way to improving that quality of life for those we hold dear and help us grieve.”
Advance Care Planning is the phrase used for people to plan their future care needs and support, including medical treatment, while they have the capacity to do so.
While doctors and other health and social care professionals are there to guide people through the Advance Care Planning process, patients and their families should take ownership of this process so that their wishes are clear and documented.
In Northern Ireland, our aging population profile indicates that in the next 25 years, we could see an increase of over 30% in the numbers dying annually.
So it’s more important than ever to have that conversation on end of life planning so that the quality of life, at the end is improved.
Loretta Gribben, Nurse Consultant, Palliative and End of Life Care, Public Health Agency said: “Palliative care ensures that a person with a serious and/or progressive condition, regardless of age or condition, can have the best possible quality of life. It may be appropriate for a number of years, not just the weeks and days at the end of life. People with palliative care needs can be supported by the whole community, including primary care, hospices, hospitals and nursing homes. A more positive experience will occur when we strengthen discussions around palliative care, involving the person and those close to them.
“Talking about dying, death and bereavement is in everyone’s interests as it can help ensure that all of us can get the care and support we want, and where we want it, at the end of our lives. “Even just having a chat with family, friends or colleagues about the importance of preparing for death can change perceptions. Through being more confident in talking about dying and taking small actions to plan for the future and support each other, together we can make a big difference. Talking about death does not bring it any closer. It is about planning for life.”
The Palliative Care in Partnership programme is aimed at improving the quality of life, at the end of life. The programme provides regional direction so that everyone identified as likely to benefit from a palliative care approach can avail of appropriate services.
The Health and Social Care Board and the Public Health Agency has been working with the Department of Health and many in the voluntary sector to understand how best to take forward a societal conversation on the topic of death, dying and bereavement.
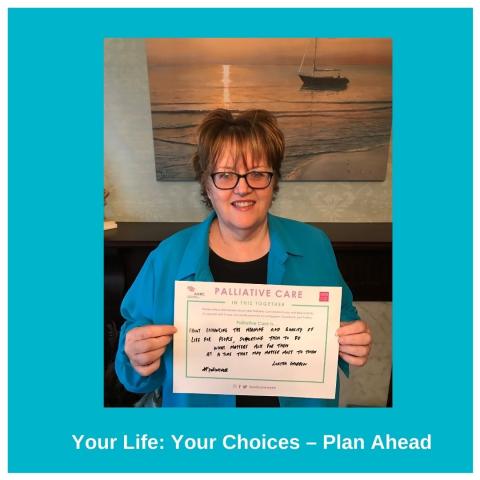
The Public Health Agency and Macmillan have produced the “Your Life: Your Choices – Plan Ahead” booklet about this process which can be downloaded from www.macmillan.org.uk
